Pelvic floor dysfunction is when the pelvic floor muscles aren't working as they should. Pelvic floor physical therapy is the go-to method for treating people with pelvic floor dysfunction.
Pelvic floor dysfunction is often underdiagnosed, and many people may have no idea that they have it. It is a common condition for women, especially after childbirth.
A report from 2022 examined the medical records of 25,425 adult females in the academic health system. 32% of the women had at least one pelvic floor dysfunction.
However, pelvic floor dysfunction can occur in both males and females. Studies suggest that 16% of men have pelvic floor dysfunction.
Men who have pelvic floor dysfunction may have urinary issues, bowel issues, or erectile dysfunction. Men may also have pain in the lower pelvic region.
The good news is that if you have pelvic floor dysfunction, you can get treatment with pelvic floor rehabilitation.
So, let's dive further into what pelvic floor dysfunction is, what can cause it, look at some ways to prevent it, and discover everything you need to know about physical therapy for pelvic floor dysfunction.
Table of Contents
- Pelvic Floor Dysfunction: The Cause for Therapy
- What Is Pelvic Floor Dysfunction?
- What Are the Causes of Pelvic Floor Dysfunction?
- Symptoms of Pelvic Floor Dysfunction
- Treatment Options for Pelvic Floor Dysfunction
- Prevention and Lifestyle Choices
- Pelvic Floor Physical Therapy
- The Goals of Pelvic Floor Physical Therapy
- How To Choose the Right Pelvic Floor Therapist for You
- Get the Therapy You Need for Your Pelvic Floor Dysfunction
Pelvic Floor Dysfunction: The Cause for Therapy
When your pelvic floor muscles, ligaments, and connective tissue are too tight or weak, it can cause bladder and bowel function issues. If you have pelvic floor dysfunction, the organs that your muscles are supporting may drop out of proper alignment and cause other bathroom-related problems.
Pelvic floor dysfunction is often treated with physical therapy. Let's take a closer look at pelvic floor dysfunction to help you better understand the signs and learn some ways that you can help prevent it.
What Is Pelvic Floor Dysfunction?
If you have pelvic floor dysfunction, then you're going to find it challenging to control your pelvic floor muscles. The inability to control your pelvic floor muscles can result in difficulty urinating, defecating, and experiencing painful sexual intercourse.
Pelvic floor dysfunction is an umbrella term that covers a multitude of issues concerning your pelvic floor region. The muscles can become either tense (hypertonicity) or loose (hypotonicity).
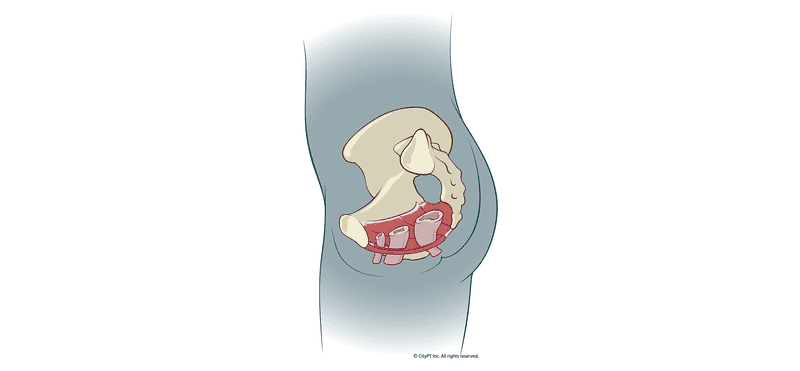
Your pelvic floor muscles support your lower pelvic region organs. If your muscles become too weak, these organs can sag or, worse, bulge out of your body. When this drop occurs, you may have a pelvic organ prolapse (POP).
Your pelvic floor muscles support the following:
- Bladder
- Rectum
- Urethra
- Large intestine
- Anus
- Vagina and uterus (female)
- Prostate (male)
These muscles not only help to support your pelvic floor but also help you use the bathroom and assist in healthy sexual function.
What Are the Causes of Pelvic Floor Dysfunction?
There can be many causes of pelvic floor dysfunction, and we're still learning possible links to pelvic floor dysfunction. Let's look at some of the most common factors.
Pregnancy and Childbirth
Women who have been pregnant are at risk for developing pelvic floor dysfunction. Simply being pregnant can lead to pelvic floor dysfunction, as pregnancy changes the pelvic area. In fact, pregnancy causes the pelvic floor to relax. Hormonal changes in women who are experiencing menopause can also change the pelvic floor tissues.
Surgery or traumatic Injury
Surgery or traumatic injuries to the pelvic region or lower back may lead to pelvic floor dysfunction. Damage to the nerves and muscles of the area can also occur from childbirth.
Aging or Being Overweight
Aging leads to hormonal, muscular, and neurological factors that may contribute to the development of pelvic floor dysfunction. Being overweight or obese is another contributing factor that may lead to pelvic floor dysfunction. Genetics
Some people are born with weaker tissues and muscles. Studies conclude that pelvic floor dysfunction is not caused by one gene alone but by multiple genes contributing to the issue.
Avoiding Using the Bathroom
Sometimes, children may avoid using the bathroom if they have had a challenging experience with learning to use the bathroom. However, holding your urine or stool in for too long can lead to pelvic floor dysfunction.
The opposite is also true if you are chronically constipated or you’re straining when you use the bathroom. These can lead to pelvic floor issues, too.
Symptoms of Pelvic Floor Dysfunction
While pelvic floor dysfunction can affect the urinary, colorectal, and reproductive systems or a combination of them all, there are some common signs and symptoms for you to be on the lookout for.
These include:
- Bathroom issues: too much or too little, straining or leaking
- Frequent, unexplainable pain in the pelvic area, lower back, or pain during sex
- Stopping and starting during urination or painful urination
If you're having any issues during "bathroom time," chances are it could be due to pelvic floor dysfunction. Most pelvic floor dysfunctions are characterized by fecal incontinence, urinary incontinence, or pelvic organ prolapse.
Treatment Options for Pelvic Floor Dysfunction
There are some ways to treat pelvic floor dysfunction. A physical therapist specializing in PT for the pelvic floor will typically provide the following treatments. Still, there are some over-the-counter or prescription medications that you can use that you'll need to see a primary care physician to get.
Pelvic floor dysfunction is commonly treated with:
- Biofeedback
- Pelvic floor physical therapy
- Medications
Biofeedback and pelvic floor physical therapy are two of the most common treatment methods if you have pelvic floor dysfunction.
Pelvic floor PT will ultimately provide you with some exercises you can learn to do at home that can help strengthen your pelvic floor muscles. If your muscles are too tense, pelvic floor PT can help you learn to relax them.
Prevention and Lifestyle Choices
According to the National Institute for Health and Care and Excellence (NICE), there are a few suggested ways to prevent pelvic floor dysfunction.
Some of these include:
- Eating a balanced diet and engaging in physical activity
- Weight loss
- Smoking cessation
- Managing chronic health issues like diabetes and chronic constipation
- Practicing pelvic floor muscle exercises (such as Kegels, which both women and men can practice)
- Participating in pelvic floor muscle training with a pelvic floor specialist
Pelvic Floor Physical Therapy
Pelvic floor therapy is a first-line method for treating most pelvic floor dysfunction. Pelvic floor rehabilitation is used to strengthen or relax the pelvic floor muscles and to reduce pain and other symptoms.
Physical therapy for pelvic floor dysfunction focuses on the fascia and muscles that surround the pelvis. A pelvic therapist has specialized training in pelvic floor dysfunction and other conditions that affect the pelvic region.
What’s Involved with Pelvic Floor Physical Therapy?
A pelvic therapy treatment plan will vary depending on your type of pelvic floor dysfunction and severity. Ultimately, we want to treat it before it gets too severe, such as certain types of pelvic organ prolapse, which may require surgery.
Once you choose your physical therapist, you'll have an initial examination where the therapist will determine what treatment will work best for you.
Often, you may benefit from many different treatments in your unique plan.
Let's look at some of the popular pelvic floor therapy options that many physical therapists use to treat pelvic floor dysfunction.
Pelvic Floor Muscle Training
Kegel exercises are a great way to build pelvic floor muscles. Adding weighted vagina cones to increase the load may also help strengthen the muscles, especially in women who find it difficult to contract the pelvic floor muscles on their own.
Practicing Kegels on your own at home is a great practice to help prevent pelvic floor dysfunction. Once you have the condition, a pelvic floor therapist can add Kegels to an overall treatment plan.
However, doing Kegels independently without a pelvic floor specialist's guidance may not change your condition. Kegels are a significant part of the treatment plan but often not the only treatment.
Manual Therapy
Manual therapy is when your physical therapist tries to relax trigger points and your pelvic floor muscles from inside of you. Your pelvic therapist can also work on the tissues outside of the body.
Manual therapy can also include myofascial release, especially if you're experiencing pain in your fascia.
Biofeedback Therapy
Biofeedback therapy uses a sensor probe that can be inserted into the vagina or the rectum that monitors the pelvic floor muscles' contractions. This allows your PT to see how well you are at contracting and relaxing them. For females, a vagina cone can be helpful with biofeedback if muscles are weak, or she can't do them on her own.
Trigger Point Therapy
Trigger point therapy uses thin needles with steroids and local anesthetic on the tip that goes into the tense knotted muscles and helps to relieve the pain and improve function.
Electrical Stimulation
Electrical stimulation is a pain-free procedure that sends a low electrical current through the pelvic floor to stimulate the muscles to contract, which ultimately helps to strengthen them.
Dry Needling
Dry needling is like trigger point therapy but uses no medication. The needle is "dry" and targets painful knotted areas to relieve pain and improve the function of the muscles. Electrical stimulation can also be added in conjunction with dry needling to enhance the effects.
The Goals of Pelvic Floor Physical Therapy
The overall goal of pelvis therapy is to help you get back to normal function and reduce pain. Pelvic floor PT can also reduce the need for surgery or medication.
Suppose you are experiencing any pain during sex or using the bathroom. In that case, prolonged physical therapy should help to reduce pain symptoms so that you can get back to your normal routine without so much pain.
Pelvic floor rehab is not a one-and-done treatment. Your therapist will schedule a length of time that works for you. Typically, eight weeks or six months is a standard timeline for therapy. Still, your treatment plan will be unique to you, and sometimes, you could benefit from a year of physical therapy.
Your pelvic floor PT results will significantly depend on your active participation. Regardless, you should gain relief from pain, improve the function of your muscles, and enjoy a better quality of life after therapy.
How To Choose the Right Pelvic Floor Therapist for You
Pelvic floor therapy works great for pelvic floor dysfunction. Nevertheless, you want to be able to trust the person you decide to work with. Choosing a pelvic therapist for this sensitive area is essential. There are a couple of things you want to check for when you are looking for the right one.
First, you'll want to ensure the physical therapist is trained in the pelvic floor area. You'll also want to see how long the appointments are to determine if you'll be given the necessary time or feel rushed along. Since this is a vulnerable area, you will likely want to have the same pelvic floor therapist do your entire treatment plan.
At CityPT, you'll get an expert in women's pelvic health to handle all your appointments and ensure that you get the time together that you deserve to heal properly.
Get the Therapy You Need for Your Pelvic Floor Dysfunction
Pelvic floor dysfunction can disrupt the quality of your life. If left unchecked, it could even lead to you needing to have surgery. Why not work to treat the issue now before it comes to surgery?
At CityPT, our pelvic floor therapists are certified in women's pelvic health and know how to help you get your muscles working as they should.
Instead of dealing with embarrassing or painful sex or bathroom issues, reach out today to book an appointment. Together, we can help you regain control over your life.
This guide is intended for informational purposes only. We are not providing legal or medical advice and this guide does not create a provider-patient relationship. Do not rely upon this guide (or any guide) for medical information. Always seek the help of a qualified medical professional who has assessed you and understands your condition.