Have you ever experienced the discomfort of waking up after a restless night of sleep only to find a tight and painful knot in your neck or shoulder? This unwelcome surprise is known as a trigger point, a fascinating area of study in the field of muscle physiology.
Trigger points, also referred to as myofascial trigger points, are localized areas of muscle fibers that have become highly sensitive and contracted. They can be caused by a variety of factors including overuse, stress, or trauma. When these trigger points form, they can cause pain, restricted movement, and even refer pain to other areas of the body.1
In this guide, we will discuss physical therapy for trigger points and explore the latest scientific knowledge surrounding their symptoms, causes, diagnosis, treatment, and prevention strategies. By the end, you will not only have a deeper understanding of trigger points but also gain valuable insights on how to manage and alleviate their impact on your daily life.
Table of Contents
- Understanding Trigger Points
- Symptoms of Trigger Points
- What are the Most Common Causes of Trigger Points?
- Diagnosing Trigger Points
- What to Expect from Physical Therapy for Trigger Points
- What If Conservative Treatment Doesn't Work?
- Preventing Trigger Points
- Is It Time to Seek Treatment?
Understanding Trigger Points
Trigger points are small knots that form when tissues within the muscle become irritated. While we primarily think of muscles as the cause of a knot, it can also be caused by increased stiffness (and tautness) of the stronger supporting layers of the muscle, known as fascia.
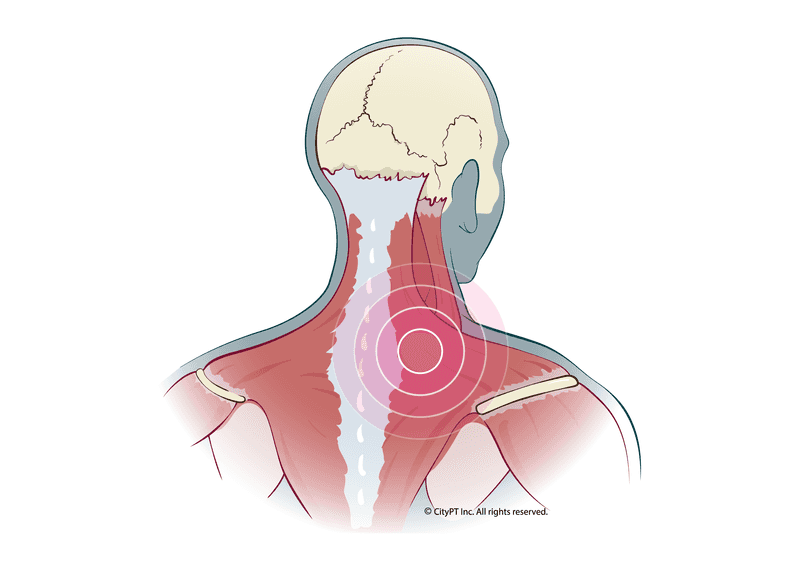
Trigger points can form in any muscle in the body, typically within the muscle belly/center. However, they are most commonly found in the shoulders, neck, and upper back.
Trigger Point Classification
There are two primary ways to classify trigger points:1
- Active trigger points: These are knots that are actively causing pain, with the pain exacerbating with touch (palpation).
- Latent trigger points: These are knots that do not cause pain but can cause stiffness in local muscles.
Additionally, a trigger point can be described as "diffuse" when there are many in one area, often due to postural abnormalities. Occasionally, trigger points can also be found in ligaments or near the tendon-muscle junctions.
Myofascial Pain vs Trigger Points
Myofascial pain is defined as pain arising from the muscles and fascia — the connective tissue surrounding your muscles. This can arise as general tenderness, aching, and fatigue as well as more specific pains such as trigger points, burning, prickling, or tingling.
A trigger point is a common type of myofascial pain. If trigger points or tenderness becomes chronic in the body, it is often classified as Myofascial Pain Syndrome. On the other hand, if there is chronic tenderness within the muscles without actual trigger points (palpable nodules), this might be classified as Fibromyalgia.2
Differentiating between the two can be difficult, requiring professional guidance to make sure you are prescribed an effective treatment program.
Symptoms of Trigger Points
Let's review symptoms associated with trigger points:3
- Severe pain with palpation: Also known as the "jump sign," active trigger points will often cause a person to wince or feel intense pain when the knot is touched.
- Referred pain: As the trigger point irritates the nerve endings around it, you may feel pain in other areas, not just where the knot is located. For example, a knot in your shoulder can cause pain to radiate up into the base of your skull.
- Weakness: Since trigger points interrupt the regular flow of signals from your brain to your muscles and cause pain, you may notice that the muscle with the trigger point is weak.
- Muscle twitching: You may see or feel your muscle jump or twitch with palpation or certain movements.
What are the Most Common Causes of Trigger Points?
There are a variety of reasons you may develop trigger points, but here are some of the most common.1
- Aging
- Postural abnormalities
- Overuse
- Joint hypermobility, instability, or other causes of joint-related pain
- Trauma
- Poor ergonomics
- Muscular imbalances/weakness
- Lack of physical activity or deconditioning4
- Poor sleep quality/quantity
- Stress (physical and emotional)
- Poor nutrition/dehydration
- Sleep disturbances
- Vitamin deficiencies
There are many theories about the mechanisms that actually cause a trigger point at a cellular level within the muscle complex. However, none have been confirmed or disproven entirely.
Diagnosing Trigger Points
If you're experiencing any of the symptoms associated with trigger points, it's important to see a doctor of physical therapy. They will perform a series of tests to determine if trigger points are the cause of your pain.
Your CityPT clinician will ask you about your symptoms, when they started, and what makes them better or worse. Then, they will perform a physical examination, including:
- Palpating for any knots or areas of tenderness/pain
- Observation of your posture and how you move to see if there are any areas of pain or restriction
- Completing a strength, flexibility, and range of motion assessment to get a sense of your overall function of the affected region
- Special tests to rule out other causes of pain, such as neck pain and back pain
What to Expect from Physical Therapy for Trigger Points
At CityPT, we personalize each patient's therapy plan based on their unique needs. Here are some examples of what treatment options you might encounter:
- Manual therapy: Including soft tissue mobilization, dry needling, myofascial release, and muscle energy techniques.
- Therapeutic exercise: To promote blood flow to affected muscle groups.
- Postural re-education and ergonomic training: To reduce unnecessary strain on local connective tissue/muscles.
- Pain relieving modalities: Such as heat, cold, electrical stimulation, and ultrasound.
- Education: To understand what is causing your trigger points, how to effectively manage them with self-care (stretching, trigger point release, etc.), and preventing future issues.
What If Conservative Treatment Doesn't Work?
If trigger points are resistant to conservative care, your clinician may recommend other treatment options such as:
- Injections: A variety of injectable agents can be used to help with trigger points, including botulinum toxin (Botox), corticosteroids, and local anesthetics.
- Medication: Such as muscle relaxants can be prescribed.
Preventing Trigger Points
Unfortunately, there is no surefire way to prevent trigger points from developing. However, there are some things you can do to lower your risk:
- Maintain good posture and alignment
- Use proper ergonomics when performing activities (and sleeping), both at work and at home
- Exercise regularly and maintain a healthy weight
- Stretch frequently, especially if you sit for long periods of time
- Manage stress with relaxation techniques such as yoga, meditation, and deep breathing
- Eat a healthy diet and stay hydrated
Is It Time to Seek Treatment?
If you're dealing with the pain and frustration of trigger points, CityPT can help. We offer a variety of services to help you find relief — both short-term and long-term. Most importantly, understanding the underlying causes of your muscle knots can be a game changer in participating in your daily activities without pain.
Book an initial evaluation today.
This guide is intended for informational purposes only. We are not providing legal or medical advice and this guide does not create a provider-patient relationship. Do not rely upon this guide (or any guide) for medical information. Always seek the help of a qualified medical professional who has assessed you and understands your condition.
References
Footnotes
-
Physiopedia. Trigger Points. Physiopedia.com Accessed November 11, 2022. https://www.physio-pedia.com/Trigger_Points ↩ ↩2 ↩3
-
Brezinschek HP. Mechanismen des Muskelschmerzes : Bedeutung von Trigger points und Tender points [Mechanisms of muscle pain : significance of trigger points and tender points]. Z Rheumatol. 2008 Dec;67(8):653-4, 656-7. German. doi: 10.1007/s00393-008-0353-y. PMID: 19015861. https://pubmed.ncbi.nlm.nih.gov/19015861/ ↩
-
Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. American family physician. 2002 Feb 15;65(4):653-62.https://www.researchgate.net/profile/Pamela-Rockwell/publication/11490100_Trigger_points_Diagnosis_and_management/links/56092b7708ae840a08d364aa/Trigger-points-Diagnosis-and-management.pdf ↩
-
Vázquez Delgado E, Cascos-Romero J, Gay Escoda C. Myofascial pain associated to trigger points: a literature review. Part 2: differential diagnosis and treatment. Medicina Oral, Patología Oral y Cirugia Bucal, 2010, vol. 15, num. 4, p. 639-643. 2010 Jul 1. http://diposit.ub.edu/dspace/handle/2445/49851 ↩