Do you suffer from foot or ankle pain? If so, you're not alone. Millions of people struggle with foot and ankle pain every day. In many cases, foot and ankle pain can be treated with physical therapy. In this article, we will discuss symptoms, causes, treatments, and how to prevent the onset of pain. Plus, we'll cover what to expect from physical therapy for foot and ankle pain.
The average adult takes anywhere from 4,000 to 18,000 steps a day, equating to 1.5 to 10 miles of walking.1
All the time spent on your feet is generally great for both your foot health and general health. However, the onset of pain can quickly make it hard to participate and enjoy even the most basic tasks of your day, such as standing to chat with a friend or walking to the mailbox.
Table of Contents
- Understanding Foot and Ankle Pain
- What Are the Most Common Causes of Pain?
- How to Diagnose Ankle and Foot Pain
- Treatment Options for Foot Pain or Ankle Pain
- Simple Exercises to Try for Foot and Ankle Pain
- How to Prevent Pain of Foot or Ankle
- Is It Time to Get Treatment for Your Ankle and/or Foot?
Understanding Foot and Ankle Pain
The foot and ankle provide a few primary functions for the body, including:
- Weight-bearing
- Forward propulsion
- Balance
Ultimately, they help us stay active in the world around us via walking, running, dancing, jumping, and so much more. The design of our feet is what makes us so unique from most mammals that get around on four limbs.
No matter what the cause, foot and ankle pain can be debilitating. If you are suffering from this type of pain, it is important to gain an understanding of what is going on.
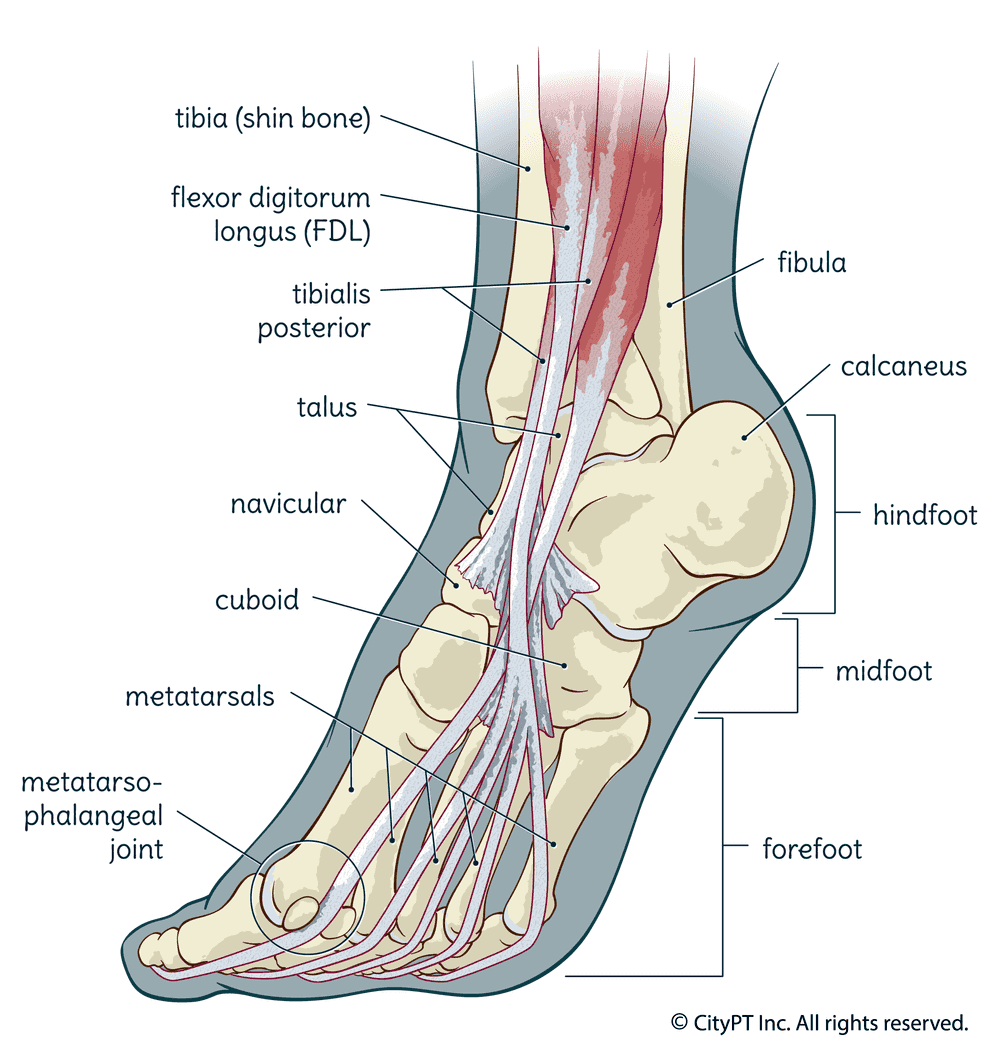
Anatomy of the Foot and Ankle
There are 28 bones in the foot and ankle, making up around a quarter of all the bones in the body in one small space. These bones connect to create purposeful joints, along with surrounding connective tissue, that allow them to function at their full potential.
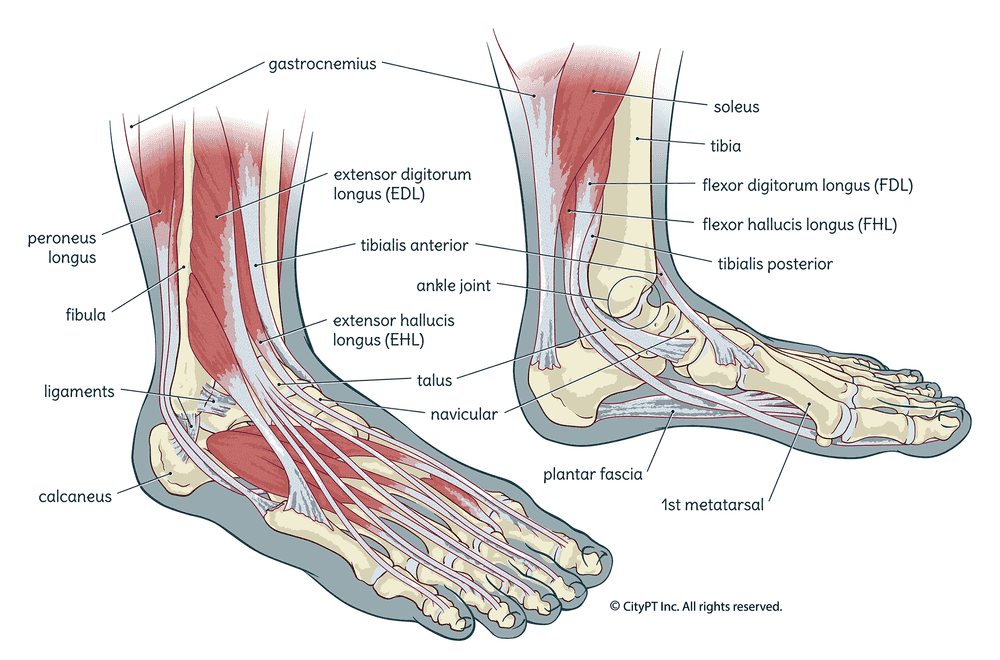
Let's review some basic foot and ankle anatomy.2
Bones
- Tarsals: The 7 bones that create the heel and base of the foot include the calcaneus (heel), talus, cuboid, navicular, and 3 cuneiforms (lateral, middle, medial). They are responsible for accepting and transferring weight across the foot.
- Metatarsals: These are the long bones in the middle of your foot that connect to your toes. They help provide leverage and support for daily activities.
- Phalanges: These are the bones in your toes. There are 14 bones total.
- The ankle joint: It is formed by the tibia and fibula (the long bones in your lower leg) connecting with the talus.
Muscles
The muscles in the foot and ankle can be divided into two main groups:
- Intrinsic: These are the small muscles within the foot that help with fine motor control. These include the muscles within the arch of your foot.
- Extrinsic: These are the larger muscles that originate outside of the foot and ankle and insert into the bones to create movement. These include the calf muscles (gastrocnemius and soleus), the peroneals (longus and brevis), and the tibialis muscle groups (anterior and posterior).
Symptoms of Foot and Ankle Pain
There are a variety of symptoms that can be associated with foot and ankle pain. Pain can range from achy to sharp and focal to generalized. It often starts as acute pain and can turn into chronic pain, if not properly addressed, over time. Some other common symptoms include:
- Swelling
- Tenderness to touch and pressure
- Bruising
- Stiffness
- Limited range of motion
- Pain with weight-bearing or walking
- Changes in sensation, such as numbness and/or tingling
- Pain at certain times of the day (such as the first step in the morning or at the end of the day)
If you are experiencing any of these symptoms, it is important to seek medical attention. A healthcare professional will be able to properly diagnose the cause of your pain and develop a treatment plan that is best for you.
What Are the Most Common Causes of Pain?
Have you asked yourself, why do I have foot pain? Many different conditions can lead to foot and ankle pain. Some of the most common causes include:
Arthritis
There are two primary types of arthritis. Osteoarthritis (OA) is a degenerative joint disease that occurs most commonly when cartilage undergoes normal age-related changes. This can be due to overuse, age, or a previous injury and may or may not be relevant to the pain presentation.
In contrast, inflammatory arthritis — such as rheumatoid arthritis and gout — is the result of systemic swelling and pain that can affect any joint in the body.
Fractures
A break in one or more of the bones in the foot or ankle can occur due to trauma, overuse (known as a stress fracture), or bone disease, such as osteoporosis. The most common sites for stress fractures include the metatarsals (the base of the toes).3
Bone Spurs
Bone spurs are bony outgrowths that can form on the joints or bones. They are often a result of degenerative joint diseases and/or overuse. They can put extra pressure where they develop, causing tenderness and altered mechanics. However, some bone spurs cause little to no pain at all.
Sprains
Ankle sprains are a tear or overstretching of the ligaments (the tissues that connect bones). This can occur due to trauma, repetitive motion, or sudden changes in direction. One of the most common sites for an acute sprain is the outer ankle.
Turf Toe is another type of sprain that occurs in the joint where the big toe meets the foot, also known as the metatarsophalangeal joint or MTP joint.
Muscle Strains
A strain is a stretched or torn muscle or tendon (the tissue connecting muscle to bone). These types of injuries often lead to swelling, bruising, and pain with movement. They typically occur due to overuse or a sudden change in activity.
Tendonitis
Tendonitis is inflammation or irritation of a tendon. Overuse, repetitive motion, and altered mechanics can all play a role. Achilles tendonitis and posterior tibialis tendinitis or tendinopathy are the most common forms.
Tendinosis
Tendinosis is a degenerative condition of the tendons. It is often due to overuse or age. Metabolic factors like diabetes can contribute to tendinosis as well.
Plantar Fasciitis
Plantar fasciitis is an inflammation of the plantar fascia (the connective tissue on the bottom of the foot). It can be caused by overuse, tightness in the calf muscles, or changes in activity level. Interestingly, plantar fasciitis may be an overused term for any heel pain, and can be mimicked by posterior tibialis tendinopathy.
Autoimmune Diseases
These are diseases that compromise tissue health, including rheumatoid arthritis or lupus.
Metatarsalgia
Metatarsalgia is a general term used to describe pain in the metatarsal region (the balls of the feet). It can be caused by many different conditions, including calluses, bunions, Morton’s neuroma, gout, and more.
Morton's Neuroma
Morton's neuroma is an enlargement of the nerve between the third and fourth toes, often caused by prolonged compression and irritation of the nerve. It can be caused by wearing tight shoes, overuse, or injury.
Calluses
Calluses are thickened areas of skin that form due to friction or pressure. They often develop on the bottom of the feet, especially under the metatarsals- and can become painful over time.
Bunions and Other Toe Malalignment
Bunions involve the enlargement and changes in the alignment of the joint at the base of the big toe. Deformities of the foot can be caused by genetics, shoes that are too tight, poor weight-bearing mechanics, arthritis, or overuse. Other common deformities include claw toe, hammer toe, and mallet toe.
Ergonomics, Posture, and Alignment
Poor ergonomics (the way we set up our home and workspace), posture, and alignment can cause repetitive stress injuries. Examples include poorly fitting shoes and sitting with the toes down/heels up. These can lead to conditions such as bursitis, tendonitis, nerve entrapment, or muscle strains.
Chronic Conditions
Chronic conditions are health conditions or illnesses that can affect blood circulation, nerve integrity, and tissue health, such as diabetes and gout.
Other Contributing Factors Include:
- Obesity or being overweight
- Chronic disease management
- Activity level
- Overall lifestyle choices related to smoking, sleep, diet, etc.
Since a lot is going on in a small space in the feet and ankles, often more than one of these issues occurs simultaneously.
How to Diagnose Ankle and Foot Pain
If you're dealing with pain, you have probably asked "When should I see a medical professional about foot or ankle pain?" The answer is, the sooner the better! Don't wait until you're limping around and miserable. Not only does limping affect the mechanics of your entire body, but foot pain has also been correlated to balance deficits that can put an individual at a higher risk for falls as they age.4
If you're ready for some answers, there are healthcare providers that will help you on your journey to proper pain management and recovery. The right diagnosis will give you some answers and get you started on the right foot (yes, pun intended!).
While you have a few different options, like your primary care physician (PCP), an orthopedic doctor, or a podiatrist, a physical therapist is specially trained to help you find the cause of your foot and ankle pain and regain function. This will help you to get back to your normal life doing the things you love as soon as possible.
It All Starts with a Physical Therapy Evaluation
At your first appointment, your physical therapist will ask you questions about your pain, medical history, and lifestyle. This will help them get to know you and what's been going on. They'll ask you questions like:
- When did your pain start?
- What activities or positions make your pain worse?
- What, if anything, makes your pain feel better?
- Do you have any other medical conditions that we should know about?
- How has this been affecting your life? Your job? Your hobbies?
- What major life changes have you sustained in the past year?
They'll also perform a physical examination. This may include:
- Observing how you walk and move
- Testing your functional abilities and balance
- Testing your range of motion
- Assessing muscle strength
- Palpating (feeling) for areas of tenderness and tissue quality
- Testing for sensation changes
- Special orthopedic tests to look at tissue and joint integrity
Do I Need Imaging for Diagnosis?
In some cases, your physical therapist may refer you to your physician - specifically a podiatrist - for imaging (like an X-ray, MRI, or CT scan). Imaging can be helpful to rule out certain conditions or get more information about a problem area. However, in many cases, imaging is not necessary for diagnosis. Your physical therapist will let you know if they think you need it.
Additionally, if a systemic cause is suspected, like gout or rheumatoid arthritis, you may need blood or urine tests ordered as well.
Treatment Options for Foot Pain or Ankle Pain
What can you do to treat your foot or ankle pain? Your physical therapist will take you through a gradual process that will help you feel empowered to recover and manage your foot and ankle pain effectively.
What to Expect from Physical Therapy for the Foot and Ankle
Your physical therapist will design a personalized treatment plan with you, based on the results of your evaluation. Treatment may include:
-
Education: Your physical therapist will teach you about your condition and what you can do to help manage your pain. This is the most powerful tool you will encounter during your treatment sessions. Understanding what is going on with your body and how to make measurable changes will help you make sustainable steps forward.
-
Modalities: Your PT care provider may use modalities like heat, cold, electrical stimulation, or ultrasound to help you manage your pain. These passive, short-term treatment options may be utilized initially if your pain is high and you are having a hard time tolerating activity. However, these should never be the primary focus of your treatment since they yield no long-term benefits.
-
Manual therapy techniques: A physical therapist can use their hands to help release any tightness or restrictions in the tissues around your foot and ankle. This may include techniques like massage, [trigger point](/guides/trigger-points/) release, myofascial release, and/or joint mobilizations. While these can be a great adjunct to other treatments, since it is a passive treatment, it isn't always necessary or the primary focus of treatment.
-
Ergonomics/posture: Many times, foot and ankle pain can be aggravated by how your body is positioned while you stand, sit, or sleep. Your PT provider will assess your posture and ergonomics (how you use your body during activities) to make sure they aren't contributing to your pain. They may also provide guidance on changes you can make at work or home to help you move better and feel better. This might include better shoe wear and orthotic recommendations. They may also recommend an orthotist for custom orthotics as needed.
-
Lifestyle: Often, our lifestyle choices can contribute to the onset of pain. Maybe we've been sitting too much, we're not moving enough, or we've picked up a new hobby that's a little too high-impact for our feet and ankles. Regardless of the reason, your physical therapist will help you identify any lifestyle changes you may need to make to help you recover. Other important factors to consider and discuss include sleep hygiene, diet, and stress management.
-
Exercise: Movement is life. Moving the body - including your feet and ankles - with intention and balance will help you in your recovery. Your physical therapist will progress you through a series of exercises specifically designed to help you achieve your goals. These may include flexibility, strengthening, balance, or proprioceptive (joint position sense) exercises. As you get stronger and your pain decreases, you will be able to do more and progress to higher-level functional, recreational, and performance-oriented activities.
Simple Exercises to Try for Foot and Ankle Pain
If you are experiencing foot or ankle pain, there are a few simple exercises that you can try at home to help ease your symptoms. It's always best to try these under the guidance of a physical therapist first to reduce the risk of aggravation and make sure you're choosing the right ones for your unique issues.
Stretches
If your foot or ankle pain is due to tightness in the muscles and other local tissues, stretching can be a way to ease your symptoms. Some simple stretches that may help include:
- Standing calf stretch: On a step or in a lunge position
- Seated ankle range of motion: Ankle rolls, pointing the toes, etc.
- Toe range of motion: Extension and flexion (bending in both directions)
Try these stretches for 60 or more seconds throughout the day as needed. If any of them elicit pain, it's best to stop or modify them.
Strengthening Exercises
If your foot or ankle pain is due to weakness, strengthening exercises are a great starting place. Some simple strengthening exercises that may help include:
- Heel raises: Raising up onto the toes, starting with both feet and progressing to one
- Toe curls: Curling the toes under while seated or standing
- Resisted ankle range of motion: Using a band or towel to provide resistance while moving the ankle through its range of motion (pointing, flexing, Rotation and side to side)
Try these exercises for 10 to 15 repetitions and 2 to 3 sets total, each day as needed.
Functional Moves
Functional exercises are important for getting back to your normal daily routine. Thus, the moves you choose should have some carry-over to your daily movement and feel purposeful. Some examples include:
- Single leg balance: Start on a solid surface and progress to softer surfaces or moving surfaces as tolerated
- Hops: Forward, sideways, and backward, single or double leg
- Step-ups: Onto a chair, step, or curb
As with the other exercises, start with what feels comfortable and gradually progress as tolerated. Remember to listen to your body and only do what feels safe. If you're unsure about any of the exercises above or if your pain persists, it's always best to consult with a physical therapist.
How Can I Treat Foot and Ankle Pain at Home?
In addition to exercises, there are a few other things you can do at home to help ease your foot or ankle pain. These are primarily useful with an acute injury and include:
- Rest: When the body is in pain, it is trying to tell you something. Often, it is best to rest the area and allow it to heal.
- Ice: Applying ice for 15-20 minutes at a time can help reduce excessive inflammation and pain.
- Elevation: Keeping the affected foot or ankle elevated above heart level can also help reduce swelling.
- Compression: Wearing a compression sock or wrapping can help provide soothing support to the joint and help with swelling.
What If Conservative Care Doesn’t Work?
If you've tried all of the above and are still experiencing foot or ankle pain, it may be time to consider other options. You can discuss these extensively with your physical therapist. These could include:
- Injections: Such as corticosteroids or platelet-rich plasma (PRP)
- Surgery: For more severe issues that have not responded to conservative care. Options include things like tendon release, debridement (removing spurs or other damaged tissues), fusions, or joint replacements.
At this point, it's important to consult with a specialist to discuss your options and find the best treatment plan for you. Regardless, your integrative care team will take care of you and get you the attention you need to get the relief you're seeking.
How to Prevent Pain of Foot or Ankle
If you aren't experiencing foot or ankle pain yet, experience off and on again pain, or want to keep it from getting worse- here are some things to consider for prevention.
- Stay active: Have a regular stretching and strengthening routine. This will help keep the muscles and tissues around the joints flexible and strong with your daily activities.
- Weight management: Reduce strain on the lower body by keeping your body weight optimal.
- Avoid high-impact activities: Particularly if you are at risk. Or make sure you are completing exercises without excessive strain (landing softly, optimal posture, etc.)
- Wear proper footwear: This can help to reduce the risk of injury. What this looks like completely depends on your unique foot and ankle alignment, flexibility, tissue health, preferences, and more.
- Make healthy lifestyle choices: Get enough sleep, stay hydrated, eat nutrient-dense foods, avoid processed foods, and practice regular stress management when possible- your feet (and entire body and mind) will thank you!
- Talk to a physical therapist: If you have any concerns or want a professional opinion on exercises, footwear, or risk of injury, please make an appointment!
- Manage any health conditions: The foot is particularly susceptible to complications from diseases like diabetes and arthritis. Make sure you are properly managing these with the guidance of your physician and with prescribed medications or lifestyle choices.
Is It Time to Get Treatment for Your Ankle and/or Foot?
If you are still experiencing pain after trying these conservative treatments at home, it may be time to seek professional help. Or if you're not sure where to start, it's time to work with a movement expert. A physical therapist can create a custom plan to ease your pain and get you back on your feet.
Schedule an appointment with one of our experts today to get started. They'll work with you to find the root cause of your pain and get you on the path to recovery.
This guide is intended for informational purposes only. We are not providing legal or medical advice and this guide does not create a provider-patient relationship. Do not rely upon this guide (or any guide) for medical information. Always seek the help of a qualified medical professional who has assessed you and understands your condition.
References
Footnotes
-
Stantos-Longhurst, Adrienne. How Many Steps Per Day to People Take on Average? Healthline.com. Published November 27, 2018. Accessed May 25, 2022. https://www.healthline.com/health/average-steps-per-day ↩
-
Physiopedia. Ankle Joint. Accessed May 26, 2022. Physiopedia.com. https://www.physio-pedia.com/Ankle_Joint ↩
-
OrthoInfo. Stress Fractures of the Foot and Ankle. Orthoinfo.aaos.org. Accessed May 26, 2022. https://www.healthline.com/health/average-steps-per-day ↩
-
Hirase PhD, PT, Tatsuya; et al. Pain Is Associated With Poor Balance in Community-Dwelling Older Adults: A Systematic Review and Meta-analysis. Journal of the American Medical Directors Association. Volume 21, Issue 5, May 2020, Pages 597-603.e8. https://doi.org/10.1016/j.jamda.2020.02.011 ↩
