In the 21st century, over 1/4 of the world population will experience disabling pain in their lower back during their lifetime. Half will experience pain for two weeks or more. Plus, an estimated 8% of the working population will be disabled each year due to low back pain.1
Thankfully, most low back pain cases will resolve within a few weeks (around six weeks). However, there are still a lot of questions to consider such as:
- What about the percentage of people that don't recover and develop chronic pain?
- What quality of life is maintained during those six weeks?
- What about the risk of future flares if the true cause of pain isn't well understood?
We'll discuss these important questions and illustrate why physical therapy is an excellent evidence-based option for understanding your injury and getting you the relief you need. Let's dive into a full guide to physical therapy for lower back pain, also known as lumbago or low back pain, to help you understand why you should book an appointment with a CityPT physical therapist as soon as possible.
Table of Contents
- Understanding Lumbago (Lower Back Pain)
- Symptoms of Low Back Pain
- What Are the Most Common Causes of Lower Back Pain?
- Acute vs. Chronic Low Back Pain
- Risk Factors for Developing Low Back Pain
- How to Diagnose Low Back Pain
- Treatment Options for Lumbago
- Exercises to Try at Home
- How to Prevent Lower Back Pain
- Do You Need PT for Low Back Pain?
Understanding Lumbago (Lower Back Pain)
Lumbago is a general term used to describe lower back pain, which can be caused by a variety of underlying issues. Unfortunately, low back pain (LBP), particularly chronic pain, is often stigmatized or written off by health professionals due to vague symptoms and unclear protocols for effective treatment.
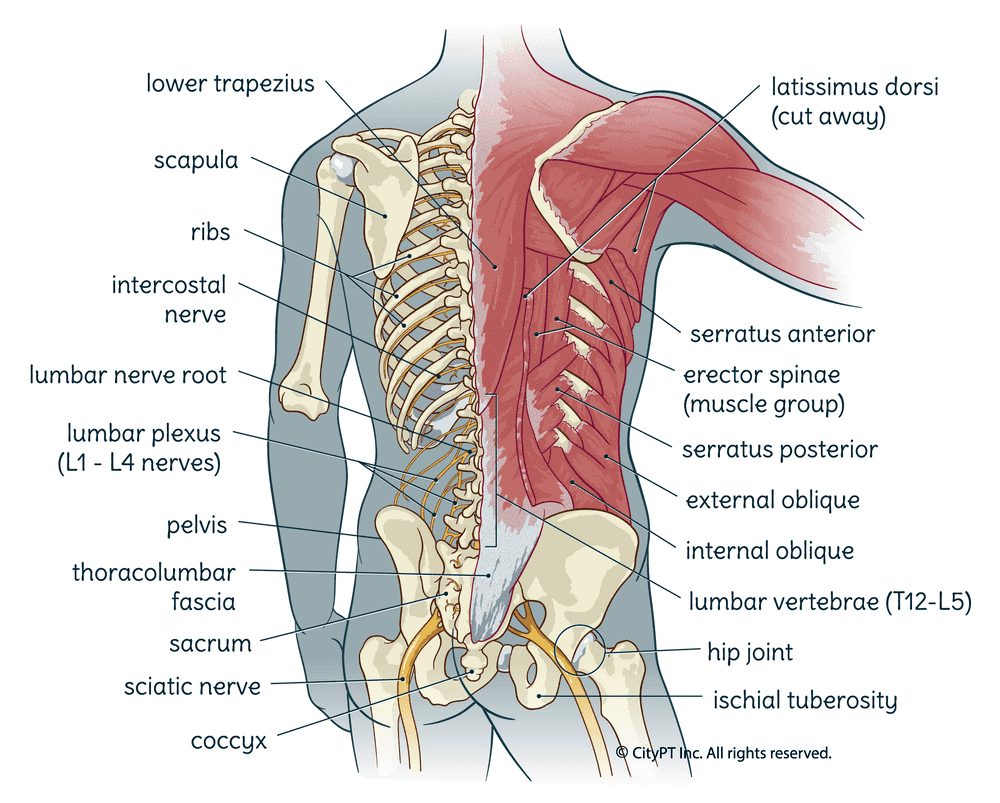
The Lumbar Spine
The lumbar spine, also known as the low back, is comprised of 5 vertebrae (L1-L5). Each vertebra is stacked on top of the other and separated by a disc. These discs act as shock absorbers to dissipate the forces placed on your spine with activities of daily living or during exercise. The vertebrae and discs are connected by a series of joints, ligaments, and muscles that work together to provide support and movement.
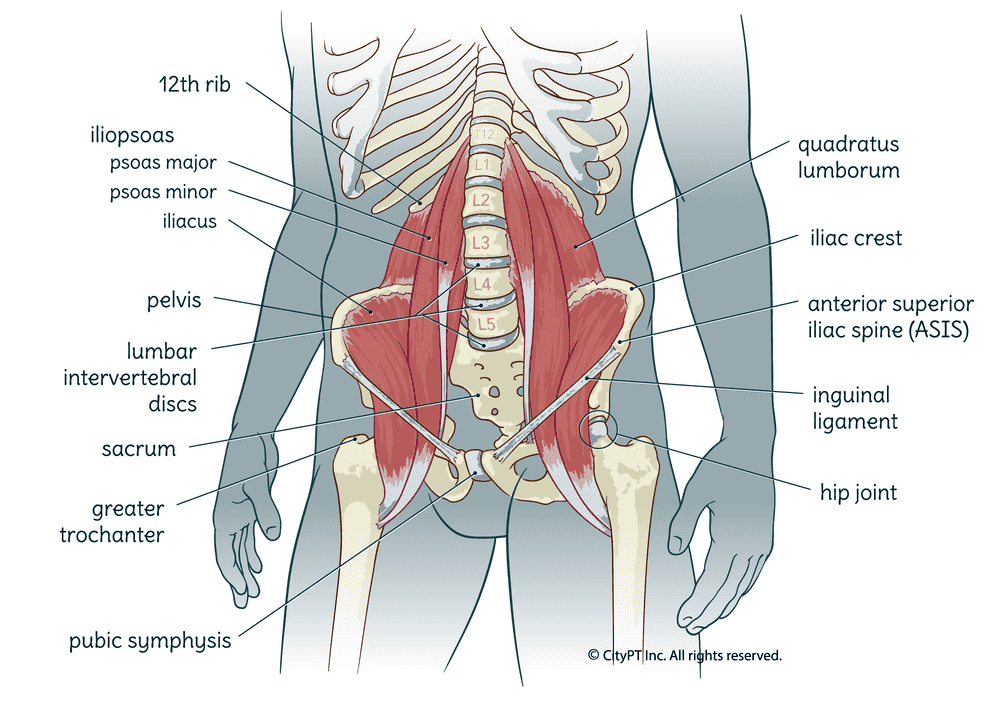
The low back has many important functions. Not only does it house the lower spinal cord and nerve roots that innervate the lower body, but it also provides some protection for our internal organs. Finally, it also plays a pivotal role in stabilizing the body to be able to move meaningfully. It's why we call the area where the low back, and associated tissues, are located the "core."
When this large area gets out of balance, it can have a serious effect on daily life.
Symptoms of Low Back Pain
The symptoms of lower back pain can vary depending on the underlying cause. However, some common signs and symptoms are associated with this condition. These include:
- Acute vs. chronic pain
- Sharp, stabbing (a sudden jolt) or dull achy pain
- Localized pain (easy to pinpoint) vs. broad pain (vague)
- Pain that is worse when you move or stand up vs. sit or lie down
- Pain that is worse when you sit or stand too long
- Muscle spasms or cramping in your lower back or legs
- Stiffness or muscle tension in your lower back
- Difficulty standing up or walking
- Radiating pain or numbness that moves down your legs, also known as referred pain, typically in a predictable pattern
- Bowel or bladder dysfunction
If you are experiencing any of these symptoms, particularly the bottom three (radiating pain, bladder/bowel changes, or a severe change in overall function), you may have more serious back issues that require medical attention. In cases like this, it's important to consult with a healthcare professional immediately to determine the underlying cause. Later, we'll discuss how physical therapists are specially trained to assess and treat conditions that cause pain and movement restrictions in the lower back.
What Are the Most Common Causes of Lower Back Pain?
Many different conditions can cause or contribute to lower back pain. Some of the most common include:
Degenerative Disc Disease (DDD)
Degenerative disc disease is a subset of normal age-related changes which appear on imaging as loss of adequate cushioning of the discs and resultant changes in the bone where the discs attach.
Herniated Disc
A herniated disc occurs when the outer layers of a disc become weak or even tear in severe cases. This herniated disc causes the bulging or leaking tissue to put pressure on local delicate tissues, including nerves, which often leads to low back pain with radiating symptoms.
Osteoarthritis
Osteoarthritis is a degenerative condition caused by the breakdown of cartilage in the joints, including the intervertebral joints (where the discs are located) and facet joints. It can lead to pain, stiffness, and inflammation in the low back — but not always.
Spinal Stenosis
Spinal Stenosis is a condition in which the spinal canal or openings for nerve roots narrow, putting pressure on the spinal cord and/or nerve roots. Spinal stenosis is often caused by degenerative changes in the spine related to aging or arthritis.
Ankylosing Spondylitis
This is a form of arthritis that primarily affects the spine. It can cause inflammation, pain, and stiffness in the lower back. Ankylosing spondylitis typically starts in the sacroiliac joints.
Compression Fractures
Compression Fractures are most commonly seen in individuals with osteoporosis (a loss of bone density) but can occur due to trauma as well. The vertebra can collapse and compress, which may lead to pain in the low back or even height loss.
Facet Joint Syndrome
The facet joints are the small joints on the back of each vertebra that allow for movement in the spine. When these joints become inflamed or irritated, it's called facet syndrome. These joints can also become stiff and arthritic over time as well.
Muscle Strain
Muscle strain is a common cause of low back pain, particularly in individuals who participate in activities that require repetitive motions or heavy lifting. The back muscles and/or tendons can become overstretched or torn, leading to inflammation, muscle tension, muscle spasms, and pain.
Sacroiliac Joint Dysfunction
The sacroiliac (SI) joints are located in the low back where the tailbone (sacrum) meets the pelvic bones (ilium). There is little movement in the SI joints themselves. The ligaments that support them become painful when they are inflamed due to injury, repetitive strain, childbirth, or muscle imbalance.
Pregnancy
Changes in tissue extensibility (due to hormones) and weight distribution (due to the growing baby) can lead to low back pain during pregnancy. Common pregnancy complaints include sciatica and SI joint dysfunction.
Radiculopathy
Radiculopathy is a condition caused by compression, inflammation, and/or injury to a nerve root in the spine. It can occur at any level of the spine and lead to pain, numbness, and weakness in the low back or legs. One of the most common conditions that can cause radiculopathy is a herniated disc.
Sciatica
Sciatica is a form of radiculopathy that specifically involves compression of the sciatic nerve. The sciatic nerve runs from the low back, through the buttocks, and down the back of the legs. Compression can lead to pain, numbness, and weakness in the low back or legs.
Non-specific Low Back Pain
This is the most common type of low back pain, accounting for 90% of all cases. It is often described as dull, achy, and/or diffuse (spread out). The exact cause is unknown but may be related to muscle strain, pregnancy, trauma, postural strain, or other factors.2 Because the innervation of many tissues in the back overlap, it can be difficult to pinpoint just one cause. Other medical conditions, such as kidney stones, endometriosis and cancer can also cause pain.
While this is not an exhaustive list, it does cover some of the most common conditions that can cause low back pain. As you can see, many different medical conditions can lead to pain in this area. It's important to consult with a healthcare professional to determine the underlying cause of your pain so that you can get the appropriate lumbago treatment.
Acute vs. Chronic Low Back Pain
It is important to note that not all lower back pain is the same. Aside from determining one or more of the causes we discussed above, this condition can be classified as acute or chronic.
Acute Pain
Acute low back pain is defined as pain lasting less than six weeks. This type of pain is usually caused by a muscle strain or other injury to the soft tissues of the back. Most people with acute low back pain will recover with conservative lumbago treatment, such as rest, ice, gentle exercise, and over-the-counter pain medication. However, once they've experienced pain, they are more likely to experience subsequent and recurrent flares.3
Chronic Pain
Chronic low back pain is defined as pain lasting more than six weeks. While it may begin acutely from the causes listed above, it turns into a complex issue due to pain receptor dysfunction, changes in brain perception, and the involvement of psychological factors.4 This is what makes the biopsychosocial approach so important for addressing this type of pain.
Additionally, you can experience "acute on chronic" pain as well. This simply means that you've flared up a chronic condition or injury.
The Ambiguity of Low Back Pain
One of the most frustrating things for low back pain sufferers is that it's often difficult to pinpoint the exact cause. This is because there are so many different structures in this area, including bones, muscles, tendons, ligaments, spinal nerves, and discs. Generalized, "one size fits all" treatment approaches to low back pain can lead to frustration, lost time, and unnecessary suffering. We will discuss how physical therapy can combat this below.
Risk Factors for Developing Low Back Pain
Some of the following factors are better supported in the literature than others.5 However, most medical providers agree that these can play a role in the development of low back pain.
- Being overweight or obese
- Smoking
- Chronic stress/anxiety
- Physical inactivity
- Repetitive motions or postures that strain the spine
- Poor biomechanics with daily activities like lifting and reaching
- Age
- Past injuries or trauma
- Genetics
- Presence of chronic inflammatory diseases, such as diabetes
- History of surgery in the abdominal region
- Pelvic floor dysfunction
How to Diagnose Low Back Pain
A thorough history and physical examination are essential for the proper diagnosis of lower back pain. Your physical therapist will ask you questions about your symptoms, medical history, and any other factors that may be contributing to your pain. They will also perform a physical examination to assess:
- Tissue palpation to determine what area is eliciting pain symptoms
- Range of motion and flexibility
- Muscle strength
- Movement patterns and coordination with daily activities
- Tissue quality, such as tender points, stiffness, warmth, etc.
- Neurological exams, such as reflexes and sensation
- Special tests to determine specific causes of low back pain
- Your pain beliefs
- Lifestyle factors
- Any other information relevant to your condition
Once the diagnosis is made, your physical therapist will work with you to develop a plan of care.
In some cases, additional testing, such as an x-ray or MRI, may be necessary to confirm the diagnosis or rule out specific causes.
You Are Not Your MRI
Sometimes an MRI can help rule out more sinister causes of low back pain, such as a tumor or severe spinal cord compression. Plus, it can paint a picture of which tissues are specifically being affected. However, it's important to take your imaging results with a big grain of salt. Whatever your MRI shows, don't get caught up in the details since it may not correlate to your symptoms or quality of life.
The truth of the matter is that some people are walking around with imaging evidence of disc issues, such as a degenerative disc disease or a herniated disc, that they'll never know about because they don't have any symptoms. On the other hand, some sufferers of acute or chronic low back pain — even severe pain — may have a "normal" MRI.6
Treatment Options for Lumbago
There are quite a few options to choose from when it comes to low back pain. We will review them all below, starting with the most effective non-surgical and conservative options.
What to Expect from Physical Therapy for Lower Back Pain
Physical therapy (PT) is an effective lumbago treatment option for most people with lower back pain. In fact, the American Physical Therapy Association (APTA) recommends PT as the first line of treatment for this condition. In particular, professionally guided and personalized exercise is effective for preventing and managing low back pain.7
Lumbago treatment options might include the following:
- Education: Your PT care provider will give you all the knowledge you need to make a successful recovery. They will help you understand the cause of your pain, what needs to be done to allow tissue healing, pain management tools to reduce sensitivity, and how to make long-term progress, and beyond. This allows you to be an active participant in your care!
Did you know that focusing on empowering education is much more effective than a passive short-term approach?
-
Exercises: Your physical therapist is a movement expert. They will work with you to prescribe specific exercises to help reduce pain, restore function and mobility, and prevent future episodes of pain. These may be done in the clinic, at home, or in a gym setting. The type and intensity of exercises will be based on your individual needs and goals.
-
Ergonomics/posture: Many people with lower back pain benefit from learning how to move their bodies in a way that reduces tissue strain, such as posture training, ergonomics review, and biomechanical training with activities of daily living, sport, and hobby. This can help to prevent future episodes of pain.
-
Modalities: Your physical therapist may use physical modalities such as heat, cold, ultrasound, or electrical stimulation to help reduce pain and inflammation. These can provide temporary pain relief and reduce the need for pain medications but are not the focus of a comprehensive treatment program.
-
Manual Therapy: If needed, your therapist can use their hands to provide temporary pain relief and restore normal function to the spine and surrounding tissues. This may include techniques such as myofascial release, trigger point dry needling, or joint mobilization/manipulation.
-
Lifestyle: Your PT care provider can help you in setting up goals and building habits related to factors like diet, exercise, sleep, and stress management. These are all important factors in overall health, tissue healing, pain coping, and well-being!
Exercises to Try at Home
The following exercises are generally safe for most people with low back pain. However, if you have any pain, particularly radiating pain, with these exercises, stop and speak with your physical therapist or physician before continuing. Starting an exercise program for low back pain without a true understanding of your pain, aka DIY PT, can lead to risks like further injury and lost productivity.
Yoga Poses to Boost Spine Flexibility
Cat-Cow:
Great for overall spine flexibility and relaxation if it can be done pain-free.
- Start on all fours with your hands under your shoulders and your knees under your hips.
- As you inhale, arch your back and look up toward the ceiling.
- As you exhale, round your spine and tuck your chin toward your chest.
- Repeat this sequence 15 to 20 times daily, moving slowly and with control.
Child's Pose:
Another great stretch to promote relaxation and stretch the entire spine. If you have pain with standing or lying flat, this will feel especially great.
- Once again, start on all fours with your hands under your shoulders and your knees under your hips.
- As you exhale, sit back on your heels and lower your forehead to the ground.
- You can either keep your arms by your sides or extend them in front of you.
- Take several deep breaths here, letting your body relax into the stretch for 30+ seconds.
Other Stretches to Try:
- Hamstring (lying on your back or standing toe touches)
- Knee to chest (one or both, also lying on your back)
- "Figure 4" glute stretch (seated with the outer ankle touching the opposite knee)
Core Targeting Strengthening Exercises
Pelvic Tilts:
An excellent exercise for retraining some of the deep core muscles, such as the transverse abdominus (lower abs) and pelvic floor, that often become dysfunctional with both acute and chronic low back pain.8
- Start by lying on your back with your knees bent and feet flat on the ground.
- As you exhale, tilt your pelvis so that your low back flattens against the ground.
- Focus on tightening the lower abs and lifting the pelvic floor without bearing down or tensing the neck.
- As you inhale, return to the starting position.
- Repeat for 10 to 15 repetitions, being sure to move slowly and with control throughout.
Plank:
This advanced movement is great for the whole body and can be easily modified for whatever level you can currently tolerate.
- Start in a push-up position with your hands under your shoulders and your feet hip-width apart.
- Keep your abs tight and spine neutral (not overly arched or flat) and hold the position- either on your hands or elbows.
- Breathe as you hold this position for 30-60 seconds.
- If this is too difficult, drop down to your knees and hold the plank position from there.
Other Core Exercises to Try:
- Dead bugs
- Seated or standing pelvic tilts
- Bridges
- Bird dogs
- Straight leg raise
- Side planks
- Prone (stomach) superman
Functional Core Strengthening Exercises
Balance - Single Leg Activities:
These exercises help to improve balance and coordination while also strengthening the deep stabilizing back muscles (of the spine).
- Start by standing on one leg with your knee slightly bent.
- If needed, hold onto a counter or chair for balance- be safe but also challenge yourself.
- Hold your balance for 30+ seconds for 2 to 3 sets on each leg.
- When you're ready, you can progress in a variety of ways- including leg lifts (side, back, or front) or standing on a softer surface (foam or carpet).
Dynamic Reaching Activities:
These exercises also help to improve the coordination of deep stabilizing back muscles with daily activities.
- Start by standing tall with your feet hip-width apart.
- Slowly reach one arm up overhead and to the opposite side.
- Focus on moving gracefully and with a feeling of strength.
- Repeat 10 to 15 times for 2 to 3 sets on each arm.
- Progress by adding weights or reaching in a variety of other positions (sideways, backward, etc.)
Other Classic Strengthening Moves to Try:
- Lunges (forward, backward, sideways)
- Squats
- Step-ups
Alternative Nonsurgical Options
Other alternative medicine and pain management options with varying levels of evidence behind them include:
- Medications: such as epidural steroid injections, nerve block injections, facet joint injections, or pain medications (over the counter and prescribed)
- Self-care: rest, exercise, modalities, etc.
- Chiropractic care
- Acupuncture
- Massage therapy
These methods may provide short-term relief but do not provide long term answers to pain.
When Physical Therapy Doesn't Work for Low Back Pain: Surgical Options
You might be wondering: how long does physical therapy take for lower back pain? This is a complicated answer that depends on your history and pain. It's best to talk to your physical therapist about realistic expectations.
Surgical treatment is reserved for when there isn't progress being made with PT or the use short-term use of pain medications or epidural steroid injections. In addition, true neurological damage must be present, meaning there is pressure directly on nerve fibers. Surgery is never advised as an option only to relieve pain because of the risks and pain that it can cause itself.
Top surgical methods that you can discuss with a sports medicine or orthopedic surgeon include:
- Discectomy: Removal of herniated tissue
- Laminectomy: Removal of bone spurs, ligaments, and other tissue compressing spinal nerves
- Spinal decompression and fusion to stabilize affected vertebrae. This can be problematic for the vertebrae above and below the fusion, as they are now at risk for overuse.9
- Artificial disc replacement is a growing surgical alternative to fusion.10
How to Prevent Lower Back Pain
The best way to prevent lower back pain is to maintain a healthy lifestyle and avoid activities that put unnecessary stress on your back. It can often be hard to pinpoint what is "straining" your back, so don't assume that what your neighbor, friend, or grandma is doing will also work for you. What's most important is to move your body in balance, do what feels good to your body, and do it in moderation.
Here are the top factors to keep in mind for prevention:
- Physical activity: Participate in general movement and core-specific exercises consistently.
- Proper nutrition and hydration: Eat nutrient-dense food and drink water to promote tissue health and assist with any necessary healing.
- Maintaining a healthy weight: Excess weight is one of the biggest strains on your joints and connective tissue.
- Avoid unnecessary strain: Set up your car, desk, bed, etc. for optimal spinal alignment.
- Make healthy lifestyle choices: Practice stress management, nurture your mental health, get enough high-quality sleep quality, etc.
Do You Need PT for Low Back Pain?
If you found yourself scrolling through and reading this article, there's a very good chance that you will benefit from PT. Whether you have a new injury or are battling a chronic issue, a physical therapist can help you protect your spine while making measurable progress that gets you back to normal life.
Ready to get started and ditch the frustration that comes with acute or chronic low back pain? Book an appointment with a CityPT expert today. You can see them almost instantly and gain valuable insight asap.
This guide is intended for informational purposes only. We are not providing legal or medical advice and this guide does not create a provider-patient relationship. Do not rely upon this guide (or any guide) for medical information. Always seek the help of a qualified medical professional who has assessed you and understands your condition.
References
Footnotes
-
Manchikanti L. Epidemiology of low back pain. Pain Physician. 2000 Apr;3(2):167-92. PMID: 16906196. https://pubmed.ncbi.nlm.nih.gov/16906196/ ↩
-
Physiopedia. Non-Specific Low Back Pain. Accessed May 12, 2022. https://www.physio-pedia.com/Non_Specific_Low_Back_Pain ↩
-
Diletto, PT, PhD, Anthony; et al. Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability, and Health from the Orthopaedic Section of the American Physical Therapy Association. Journal of Orthopaedic & Sports Physical Therapy Published Online: April 1, 2012. Volume 42, Issue 4, Pages A1-A57. https://www.jospt.org/doi/10.2519/jospt.2012.42.4.A1 ↩
-
Jenkins, Luke; et al. Low Somatosensory Cortex Excitability in the Acute Stage of Low Back Pain Causes Chronic Pain. Journal of Pain. Volume 23, Issue 2. February 2022, Pages 289-304. https://www.sciencedirect.com/science/article/abs/pii/S1526590021003199 ↩
-
Mayo Clinic. Back Pain. Mayoclinic.com. Accessed May 12, 2022. https://www.mayoclinic.org/diseases-conditions/back-pain/symptoms-causes/syc-20369906 ↩
-
Bainska, Anna; et al. No association between MRI changes in the lumbar spine and intensity of pain, quality of life, depressive and anxiety symptoms in patients with low back pain. Neurologia i Neurochirurgia Polska. Vol 53, No 1 (2019) #61717. https://journals.viamedica.pl/neurologia_neurochirurgia_polska/article/view/61717# ↩
-
Shipton EA. Physical Therapy Approaches in the Treatment of Low Back Pain. Pain Ther. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6251828/ ↩
-
Selkow NM, Eck MR, Rivas S. TRANSVERSUS ABDOMINIS ACTIVATION AND TIMING IMPROVES FOLLOWING CORE STABILITY TRAINING: A RANDOMIZED TRIAL. Int J Sports Phys Ther. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5717480/ ↩
-
Lee JC, Choi SW. Adjacent Segment Pathology after Lumbar Spinal Fusion. Asian Spine J. 2015;9(5):807-817. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4591457/ ↩
-
Salzmann SN, Plais N, Shue J, Girardi FP. Lumbar disc replacement surgery-successes and obstacles to widespread adoption. Curr Rev Musculoskelet Med. 2017;10(2):153-159. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5435628/ ↩
