Disc herniations can lead to a variety of symptoms, depending on their location. They are most common in individuals between the ages of 30 and 50 years old.1 In this guide, we will discuss the basics of herniated discs, including symptoms, causes, diagnostics, physical therapy treatment, and prevention.
Disc herniation is only a concern when it compresses a local nerve, causing symptoms. In fact, MRIs will often show asymptomatic disc herniations.2 Conservative treatment is the recommended first step when any symptoms occur.
Table of Contents
- Understanding Disc Herniation
- Symptoms of a Herniated Disc
- Causes of Disc Herniation
- Diagnosing a Herniated Disc
- What to Expect from Physical Therapy for the Spine
- Do I Need Herniated Disc Surgery?
- How to Prevent Disc Herniation
- CityPT Modern Physical Therapy is Your Best Tool for Disc Herniation
Understanding Disc Herniation
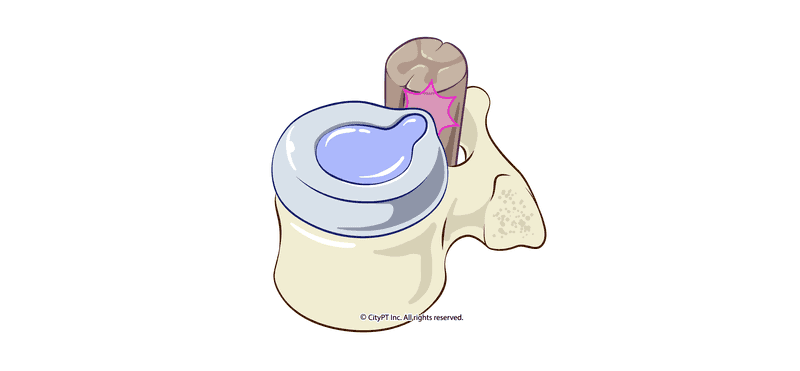
The discs in our spine act as cushions between the vertebrae. They are filled with a jelly-like substance called the nucleus pulposus.
A herniated disc occurs when the outer layer of the disc, called the annulus fibrosus, becomes compromised and causes the nucleus pulposus to be displaced. This can occur anywhere in the spine — there are 23 discs between the vertebrae. The most common site of disc herniation is the lumbar spine (low back), followed by the cervical spine (neck).2
Types of Disc Herniation
There are four stages of disc herniation: bulging, protrusion, extrusion, and sequestration. A disc herniation can gradually progress from one stage to the next or hit one stage suddenly due to trauma or sudden tissue give.
- Bulging occurs when the outer layer of the disc is damaged, causing the inner jelly-like substance to bulge out.
- Protrusion occurs when the nucleus pulposus protrudes beyond the inner layers, but not the fibrous most outer layer (layers are intact).
- Extrusion occurs when the nucleus pulposus breaks through the outer layers of the disc.
- Sequestration occurs when the extrusion is completely separate from the parent disc and is displaced in the spinal canals or epidural space.
Bulging Disc vs Herniated Disc
A herniated disc is a blanket term for the degeneration of the disc that causes the jelly-like center to change shape. A bulging disc specifically refers to the first stage, or mildest version of disc herniation — when the center bulges out, but the outer layer is still intact.
Disc Herniation and Aging
Why is disc herniation most common between 30 and 50 years of age? This is because the discs naturally lose moisture and extensibility with each decade after 30. However, once there has been significant water loss in the discs past the age of 50, then the risk of herniation drops since there is no longer substantial disc to bulge or leak.
Beyond the age of 65, the bigger concerns in the spine now involve issues like bone spurs, narrowing of the nerve root and spinal canal space, and other age-related degenerative changes that can potentially lead to pain.1
Symptoms of a Herniated Disc
The symptoms of a herniated disc will vary depending on the location of the injury and the severity of the disc damage. Most often, herniated discs do no produce any symptoms and will heal on their own.1
When symptoms are present, the most common symptom is pain, which can range from sharp to dull and achy. The pain may be localized to the area of the herniation or radiate down an arm or leg.
Other symptoms may include:
- Muscle weakness
- Numbness or tingling in the affected arm or leg
- Difficulty staying in one position for too long
- Pain that is worse in the morning, when our discs are most aqueous
- Pain with sneezing, bearing down, or coughing
- Stiffness of the spine, difficulty bending or rotating specific segments
- Radiating pain down the arm or leg
- Difficulty moving the affected arm or leg
- Loss of bowel or bladder control (in severe cases)
If you experience any of these symptoms, it is important to see a physician or spine specialist to rule out other potential causes of your pain.
In particular, if you experience "red flag" symptoms like sudden changes in bowel or bladder control, new numbness in the saddle area (where you'd sit on a bike seat), or sudden sexual dysfunction, these are all signs of cauda equina and you should seek medical care immediately.
Causes of Disc Herniation
There are a variety of causes of disc herniation. Most often, it is due to initial degenerative changes that occur around age 40.2 Other potential causes include:
- Trauma or injury to the spine
- Repetitive motions that put stress on the spine (such as excessive twisting and bending without adequate breaks)
- Obesity or extra weight around the waistline
- Holding a chronically over-flexed position of the spine
- Living a sedentary lifestyle
- Vibration of heavy machinery and truck driving
- Smoking
Diagnosing a Herniated Disc
If you are experiencing any of the symptoms listed above, your doctor might order an MRI to confirm the diagnosis — particularly if symptoms are severe and other spine conditions need to be ruled out. While this information can be helpful and guide treatment, an MRI can also show changes in the spine that are not causing any pain or other symptoms, thus leading to unnecessary concern.
What's most important with recovery from a herniated disc is diagnosing your current functional deficits. This is why a CityPT physical therapy examination is most beneficial. First, we will discuss your medical history, symptoms, lifestyle, and biggest concerns. Then, during a telemedicine or in-person consultation, will look at factors like strength, flexibility, coordination, mobility, and more.
What to Expect from Physical Therapy for the Spine
The goal of physical therapy is to help you decrease pain, improve function, and prevent re-injury for long term results. Depending on your symptoms, this might look different for everyone.
Common treatments might include:
- Manual Therapy: Hands-on treatment that can help decrease pain and muscle spasm, including soft tissue mobilization and spinal mobilization.
- Therapeutic exercises: The spine likes to move. Exercises are specifically chosen to help stabilize symptoms and function, with a focus on strengthening, flexibility, and coordination.
- Modalities: This might include electrical stimulation, heat, or cold to help decrease pain short term and allow tolerance for an exercise program.
- Education: Most importantly, you will learn about your injury, how to prevent re-injury and self-management strategies. There is typically a lot of fear and confusion surrounding back pain and disc herniation that can lead to counterproductive avoidance of normal daily activities. Having an understanding of what's actually going on and feeling confident in continued movement is a game changer.
- Discussing lifestyle factors: Habits and past experiences (trauma, emotional stress, etc) might be playing a role in your current symptoms. It can be helpful to process these things with someone who can offer guidance and support for making changes.
- Ergonomics: If your job or daily activities contribute to your symptoms, your physical therapist can assess and make recommendations for changes that will help decrease pain and improve function long term.
Do I Need Herniated Disc Surgery?
Most people with a herniated disc recover without surgery within a few weeks to months, especially with the initiation of motor control training.3 However, if you have severe neurological symptoms (such as weakness, tingling, and radiating pain) and do not respond to conservative care, you might be a candidate for surgery. You can discuss options with your physical therapist and surgeon.
How to Prevent Disc Herniation
There are a few things you can do to help prevent disc herniation:
- Manage your weight: Excess weight around the waistline puts extra pressure on the discs in your spine with daily movement.
- Quit smoking: Smoking decreases blood flow to the discs and makes them more likely to degenerate.
- Exercise: A regular exercise routine helps maintain a healthy weight, flexibility, and strength — all important for spine health. It's important to move your spine in its full range of motion and not be afraid to do so. Plus, the duration and intensity of your exercise program should be enough to offset the hours you spend sitting.
- Take breaks: Take active breaks away from your seat. This can include a bout of stretching or walking.
- Posture: Be aware of your posture throughout the day with both static and dynamic movement. When sitting, standing, walking, or lying down, keep your spine well supported to complete your activities.
- Ergonomics: If you have a job that requires sitting at a desk or standing for long periods of time, make sure you have a well-supported workstation. Take breaks often to move your body and keep the blood flowing.
CityPT Modern Physical Therapy is Your Best Tool for Disc Herniation
If you are currently dealing with a herniated disc, or think you might have one, don't hesitate to seek professional help. A CityPT physical therapist will be your best asset to get you on a path to recovery. Many people are afraid of a disc herniation diagnosis, but there's no need to feel hopeless — we understand your pain and condition, and we can help.
Get in touch with one of our CityPT spine experts to start your recovery process.
This guide is intended for informational purposes only. We are not providing legal or medical advice and this guide does not create a provider-patient relationship. Do not rely upon this guide (or any guide) for medical information. Always seek the help of a qualified medical professional who has assessed you and understands your condition.
References
Footnotes
-
Dydyk AM, Ngnitewe Massa R, Mesfin FB. Disc Herniation. [Updated 2022 Jan 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. https://www.ncbi.nlm.nih.gov/ ↩ ↩2 ↩3
-
Physiopedia. Disc Herniation. Physiopedia.com. Accessed August 15, 2022. https://www.physio-pedia.com/Disc_Herniation ↩ ↩2 ↩3
-
Pourahmadi M, Delavari S, Hayden JA, et alDoes motor control training improve pain and function in adults with symptomatic lumbar disc herniation? A systematic review and meta-analysis of 861 subjects in 16 trialsBritish Journal of Sports Medicine Published Online First: 14 June 2022. doi: 10.1136/bjsports-2021-104926 ↩